State sma Bali Mandara is a boarding school in Bali. Here we live together early in the afternoon, and evening. Many of the activities we do here. Every day, we have a very full of activities every day such as learning, makes the job dormitories, sheet making, making the task group, studying for exams, our residential cleaning, clean up our schools, and other activities that we have to do. Although we have free time like Saturday and Sunday, we still have a lot of activity on that day. Finally, all students in Smanbara experience stress. Although only the stress per se, but actually we should not underestimate, because people who are only exposed to the stress will get a disease. Stress is one of them will attack our digestive system. The effect of stress is that we will get ulcer disease. Ulcer disease is a disease that most commonly encountered on every student who was in smanbara
Gastritis or Maag
Gastritis is a condition in which the stomach lining—known as the mucosa—is inflamed. The stomach lining contains special cells that produce acid and enzymes, which help break down food for digestion, and mucus, which protects the stomach lining from acid. When the stomach lining is inflamed, it produces less acid, enzymes, and mucus.
Gastritis may be acute or chronic. Sudden, severe inflammation of the stomach lining is called acute gastritis. Inflammation that lasts for a long time is called chronic gastritis. If chronic gastritis is not treated, it may last for years or even a lifetime.
Erosive gastritis is a type of gastritis that often does not cause significant inflammation but can wear away the stomach lining. Erosive gastritis can cause bleeding, erosions, or ulcers. Erosive gastritis may be acute or chronic.
The relationship between gastritis and symptoms is not clear. The term gastritis refers specifically to abnormal inflammation in the stomach lining. People who have gastritis may experience pain or discomfort in the upper abdomen, but many people with gastritis do not have any symptoms.
The term gastritis is sometimes mistakenly used to describe any symptoms of pain or discomfort in the upper abdomen. Many diseases and disorders can cause these symptoms. Most people who have upper abdominal symptoms do not have gastritis.
Psychic or psychological factors can also increase a person’s stomach acid production. Besides ulcer disease can also be caused infection certain bacteria, such as Helicobacter pylori which is a normal bacteria in the stomach, which under certain conditions can become abnormal. Which ultimately stimulates gastric acid. Gastritis can also be caused by allergies to certain foods such as fish, chocolate and others.
• There are several stages in ulcer disease, namely:
1. Mild Gastritis
Maag still relatively mild mild stage where usually each person was at this stage, if the examination will be visible excess stomach acid in the walls.
2. Ulcer Was
Maag at this stage is causing pain, nausea and painful illness.
3. Chronic Gastritis
Chronic heartburn is heartburn that is severe gastritis compared to normal intensity.
4. Gastric Cancer
Stomach cancer caused by harmful microorganisms, namely Helycobacter pylori.
The Cause of Gastritis or Maag
Helicobacter pylori (H. pylori) infection causes most cases of chronic no erosive gastritis. H. pylori are bacteria that infect the stomach lining. H. pylori are primarily transmitted from person to person. In areas with poor sanitation, H. pylori may be transmitted through contaminated food or water.
In industrialized countries like the United States, 20 to 50 percent of the population may be infected with H. pylori. Rates of H. pylori infection are higher in areas with poor sanitation and higher population density. Infection rates may be higher than 80 percent in some developing countries.
The most common cause of erosive gastritis—acute and chronic—is prolonged use of non steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen. Other agents that can cause erosive gastritis include alcohol, cocaine, and radiation.
Traumatic injuries, critical illness, severe burns, and major surgery can also cause acute erosive gastritis. This type of gastritis is called stress gastritis.
Less common causes of erosive and non erosive gastritis include
• autoimmune disorders in which the immune system attacks healthy cells in the stomach lining
• some digestive diseases and disorders, such as Cohn’s disease and pernicious anemia
• viruses, parasites, fungi, and bacteria other than H. pylori
The symptoms of gastritis
Many people with gastritis do not have any symptoms, but some people experience symptoms such as
• upper abdominal discomfort or pain
• nausea
• vomiting
These symptoms are also called dyspepsia.
Erosive gastritis may cause ulcers or erosions in the stomach lining that can bleed. Signs of bleeding in the stomach include
• blood in vomit
• black, tarry stools
• red blood in the stool
The complications of gastritis
Most forms of chronic nonspecific gastritis do not cause symptoms. However, chronic gastritis is a risk factor for peptic ulcer disease, gastric polyps, and benign and malignant gastric tumors. Some people with chronic H. pylori gastritis or autoimmune gastritis develop atrophic gastritis. Atrophic gastritis destroys the cells in the stomach lining that produce digestive acids and enzymes. Atrophic gastritis can lead to two types of cancer: gastric cancer and gastric mucosa-associated lymphoid tissue (MALT) lymphoma.
The Gastritis Diagnosed
The most common diagnostic test for gastritis is endoscopy with a biopsy of the stomach. The doctor will usually give the patient medicine to reduce discomfort and anxiety before beginning the endoscopy procedure. The doctor then inserts an endoscope, a thin tube with a tiny camera on the end, through the patient’s mouth or nose and into the stomach. The doctor uses the endoscope to examine the lining of the esophagus, stomach, and first portion of the small intestine. If necessary, the doctor will use the endoscope to perform a biopsy, which involves collecting tiny samples of tissue for examination with a microscope.
Other tests used to identify the cause of gastritis or any complications include the following:
• Upper gastrointestinal (GI) series. The patient swallows barium, a liquid contrast material that makes the digestive tract visible in an x ray. X-ray images may show changes in the stomach lining, such as erosions or ulcers.
• Blood test. The doctor may check for anemia, a condition in which the blood’s iron-rich substance, hemoglobin, is diminished. Anemia may be a sign of chronic bleeding in the stomach.
• Stool test. This test checks for the presence of blood in the stool, another sign of bleeding in the stomach.
• Tests for H. pylori infection. The doctor may test a patient’s breath, blood, or stool for signs of infection. H. pylori infection can also be confirmed with biopsies taken from the stomach during endoscopy.
The gastritis treated
Medications that reduce the amount of acid in the stomach can relieve symptoms that may accompany gastritis and promote healing of the stomach lining. These medications include
• antacids, such as Alka-Seltzer, Maalox, Mylanta,Rolaids, and Rio-pan. Many brands on the market use different combinations of three basic salts—magnesium, calcium, and aluminum—with hydroxide or bicarbonate ions to neutralize the acid in the stomach. These drugs may produce side effects such as diarrhea or constipation.
• histamine 2 (H2) blockers, such as famotidine (Pepcid AC) and ranitidine (Zantac 75). H2 blockers decrease acid production. They are available both over the counter and by prescription.
• proton pump inhibitors (PPIs), such as omeprazole (Prilosec, Zegerid), lansoprazole (Prevacid), pantoprazole (Protonix), rabeprazole (Aciphex), esomeprazole (Nexium), and dexlansoprazole (Kapidex). All of these drugs are available by prescription, and some are also available over the counter. PPIs decrease acid production more effectively than H2 blockers.
Depending on the cause of the gastritis, additional measures or treatments may be needed. For example, if gastritis is caused by prolonged use of NSAIDs, a doctor may advise a person to stop taking NSAIDs, reduce the dose of NSAIDs, or switch to another class of medications for pain. PPIs may be used to prevent stress gastritis in critically ill patients.
Treating H. pylori infections is important, even if a person is not experiencing symptoms from the infection. Untreated H. pylori gastritis may lead to cancer or the development of ulcers in the stomach or small intestine. The most common treatment is a triple therapy that combines a PPI and two antibiotics—usually amoxicillin and clarithromycin—to kill the bacteria. Treatment may also include bismuth subsalicylate (Pepto-Bismol) to help kill bacteria.
After treatment, the doctor may use a breath or stool test to make sure the H. pylori infection is gone. Curing the infection can be expected to cure the gastritis and decrease the risk of other gastrointestinal diseases associated with gastritis, such as peptic ulcer disease, gastric cancer, and MALT lymphoma.
Foods to avoid for people who suffer from maag
1. Coffee, tea or other drinks that contain caffeine
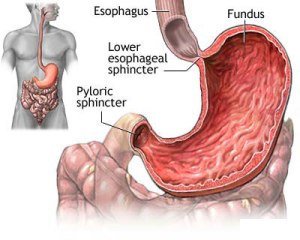
Caffeine can relax the lower esophageal sphincter (LES), the valve between the stomach and throat, causing the gas in the stomach rises up the esophagus.
2. Brown
Chocolate contains concentrations of theobromine (a compound that occurs naturally in plants such as cocoa, tea and coffee), which would relax the LES muscle, triggering stomach acid up into the esophagus.
3. Oily and fatty foods
These foods tend to be slowly digested, allowing food to stay longer in the stomach. This can produce an increase in pressure in the stomach, which in turn will increase the attenuation of LES pressure. If the LES weakens, stomach acid to rise into the esophagus.
4. Tomatoes and tomato-based products
These foods relax the lower esophageal sphincter that make up the stomach acid
5. Alcohol
Alcohol relaxes the sphincter, causing reflux, or reversal of stomach acid into the esophagus. Alcohol also increases the production of stomach acid.
6. Cigarette
The chemicals in cigarette smoke can weaken the LES as they pass through the lungs into the blood.
7. Eating in the number of
Stomach ‘full’ could provide extra pressure on the sphincter, which will increase the chances of a reversal of the incidence of food into the esophagus.
8. Acid and fruit juice
Fruits that taste following acid products, such as juice, plays a role in flexing the LES.
9. Eat between 2-3 hours before bed
Lying down with a full stomach can cause stomach contents sphincter pressure, increases the chances of reflux of food into the esophagus.
10. Clothes Too Tight
Clothes that are too tight hug around the stomach will put pressure on the stomach, so food will be driven up pushing LES valve. Clothing that can cause this kind of problem, among others, corsets and tightening the belt too tight …
how to prevent maag by always eating broccoli and bananas. Because fruits and vegetables can prevent the occurrence of maag disease.
hhe ga nyangka bisa buat artikel kaya gni juga 😀